A Clinician’s Guide to Clinical Endodontics
Course Number: 562
Course Contents
Periradicular Diagnosis
When clinicians perform restorative or endodontic treatment, they do not often obtain a periradicular diagnosis. However, making a periodontal diagnosis is especially helpful when a patient presents in pain. A study by McCarthy et al 12 demonstrated that patients presenting with periradicular pain can localize the painful tooth 89% of the time and that patients who present with tooth pain without periradicular pain can localize the tooth only 30% of the time.
By objectively testing the periradicular tissue, a dentist can best determine its gingival and periradicular status. Below are the current periradicular diagnosis terminologies.10
Normal periodontal tissue: Not sensitive to percussion or palpation testing. Also, radiographically, the lamina dura surrounding the root is intact.
Symptomatic apical periodontitis: The tooth has a painful response to biting and/or percussion. This may or may not be accompanied by radiographic periradicular changes.
Asymptomatic apical periodontitis: The tooth has no pain on percussion or palpation. Radiography reveals apical radiolucency.
Chronic apical abscess: Radiography typically reveals a radiolucency. Clinically, there is a sinus tract present on the gingival tissue. The draining sinus tract should be traced with a gutta-percha cone and then confirmed radiographically (Figure 5 and Figure 6).
Figure 5.
Clinical confirmation of the periradicular diagnosis—chronic apical abscess on tooth No. 19. The tooth is not sensitive to percussion or palpation. A gutta-percha cone is inserted into the sinus tract.
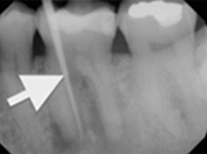
Figure 6.
Radiographic confirmation of periradicular diagnosis—chronic apical on tooth No. 19. Note the tracing of the inserted gutta-percha to the etiology. Local anesthesia is generally not required for a sinus tract tracing.
Acute apical abscess is an inflammatory reaction to pulpal infection and necrosis characterized by rapid onset, spontaneous pain, extreme tenderness of the tooth to pressure, pus formation, and swelling of associated tissues. There may be no radiographic signs of destruction, and the patient often experiences malaise, fever, and lymphadenopathy.
Condensing osteitis is a diffuse radiopaque lesion in the periapical region. The opacity represents a localized osseous reaction to a low-grade inflammatory stimulus.