Geriatric Dentistry: Before You Call 911
Course Number: 586
Course Contents
Fundamental Elements Needed to Prevent Transmission of Infectious Agents in Dental Settings: (CDC Infection Control Guidelines)
CDC also provides an Infection prevention checklist for dental settings to ensure safe care.28 The checklist can be used to:
Ensure the dental health care setting has appropriate infection prevention policies and practices in place, including appropriate training and education of dental health care personnel (DHCP) on infection prevention practices.
Ensures adequate supplies to allow DHCP to provide safe care and a safe working environment.
Systematically assess personnel compliance with the expected infection prevention practices and provide feedback to DHCP regarding performance. Assessment of compliance should be conducted by direct observation of DHCP during the performance of their duties.
Documentation
The task of creating documented infection prevention policies and procedures based on evidence-based rules, regulations, or standards should fall under the purview of at least one individual who has received training in infection prevention coordinator. 27Policies and procedures should be adapted to the dental context and regularly (e.g., annually) reevaluated in accordance with any applicable state or federal regulations.
CDC also recommends that all dental facilities establish policies and procedures for the early identification and management of potentially infected individuals at the first points of patient contact.
Create and manage programs for occupational health and infection prevention.
Educate and teach all dental healthcare staff on infection prevention practices appropriate to their jobs or tasks (DHCP)
The most recent CDC advice on vaccines, testing, and follow-up is available.
Establish a regular review process for the infection prevention program, which includes assessing DHCP's compliance with infection prevention guidelines. 82
Standard Precautions consists of:
Hand washing.
Putting on personal safety gear (e.g., gloves, masks, eyewear).
Respiratory hygiene/ cough etiquette.
Sharps safety (engineering and work practice controls).
Aseptic safe injection practices
Sterile instruments and devices.
Clean and disinfected environmental surfaces
Practice hand hygiene when:
Hands are obviously dirty.
Following barehanded contact with tools, materials, equipment, and other items that could be contaminated by blood, saliva, or respiratory secretions.
Before and after each patient's treatment.
Before putting on gloves and once more right after taking them off.
Respiratory Hygiene and Cough Etiquette
Effective respiratory hygiene and cough etiquette are essential measures to prevent the transmission of respiratory infections in healthcare settings. The following practices are recommended:
Containment of Respiratory Secretions: Respiratory secretions from symptomatic individuals should be contained immediately upon entry to the facility and throughout their visit.
Patient Education: Clear and visible signage should be displayed at facility entrances, instructing individuals with respiratory symptoms to:
Cover their mouth and nose when coughing or sneezing.
Use disposable tissues and discard them appropriately.
Perform hand hygiene after contact with respiratory secretions.
Accessibility of Hygiene Resources: Tissues and no-touch disposal receptacles should be provided in accessible locations. Hand hygiene resources, such as hand sanitizer stations or sinks, should be available in or near waiting areas.
Use of Masks: Symptomatic patients and their accompanying caregivers should be offered masks to reduce the spread of infectious droplets.
Physical Distancing: Patients exhibiting symptoms of respiratory infections should be seated as far as possible from others. Where feasible, a designated waiting area should be provided for these individuals.
Staff Education: Dental Health Care Personnel (DHCP) should receive ongoing education regarding infection prevention strategies, emphasizing the importance of containing respiratory secretions to minimize the spread of respiratory pathogens during patient care.
Personal safety should be ensured using PPE
PPE, including medical masks, gowns, goggles, gloves, and face shields, is essential for protecting healthcare workers from infections like COVID-19. Quality-assured PPE remains critical for worker safety, continuity of care, and pandemic preparedness.85 PPE with a guarantee of quality is still in high demand. In fact, as part of the COVID-19 response, UNICEF has sent more than 653.4 million PPE pieces to 140 countries since the pandemic started.29
According to CDC guidelines, Healthcare personnel should use the following PPE:
Face mask - An N95 respirator or a respirator approved under standards used in other countries that are like NIOSH-approved N95 filtering facepiece respirators Or A well-fitting facemask (e.g., selection of a facemask with a nose wire to help the facemask conform to the face).
Eye protection - Put on eye protection (i.e., goggles or a face shield that covers the front and sides of the face). Protective eyewear is required by OSHA regulations under General Industry 1910.133.a and recommended by CDC. 30
Gloves - Put on clean, non-sterile gloves upon entry into the patient room or care area. It should be removed after patient care and hands should be immediately washed. the gloves should be changed if they become torn or heavily contaminated.
Patient examination or surgical gloves should not be washed before use. Disposable gloves should not be reused.
Gowns - Put on a clean isolation gown upon entry into the patient room or area which is to be changed if it becomes soiled. DHCP should wear long-sleeved disposable or reusable gowns or lab coats that cover skin and personal clothing likely to become soiled with blood, saliva, or infectious material—for example, when spatter and spray of blood, saliva, or other potentially infectious material to the forearms might occur. DHCP should change protective clothing when it becomes visibly soiled or as soon as feasible if penetrated by blood or other potentially infectious fluids.86
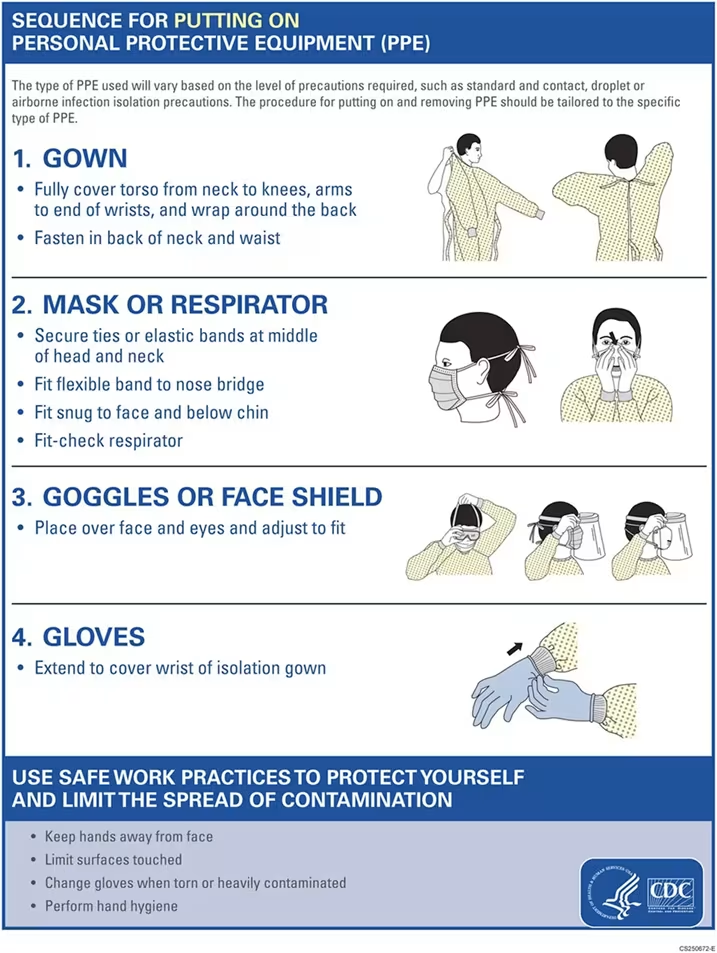
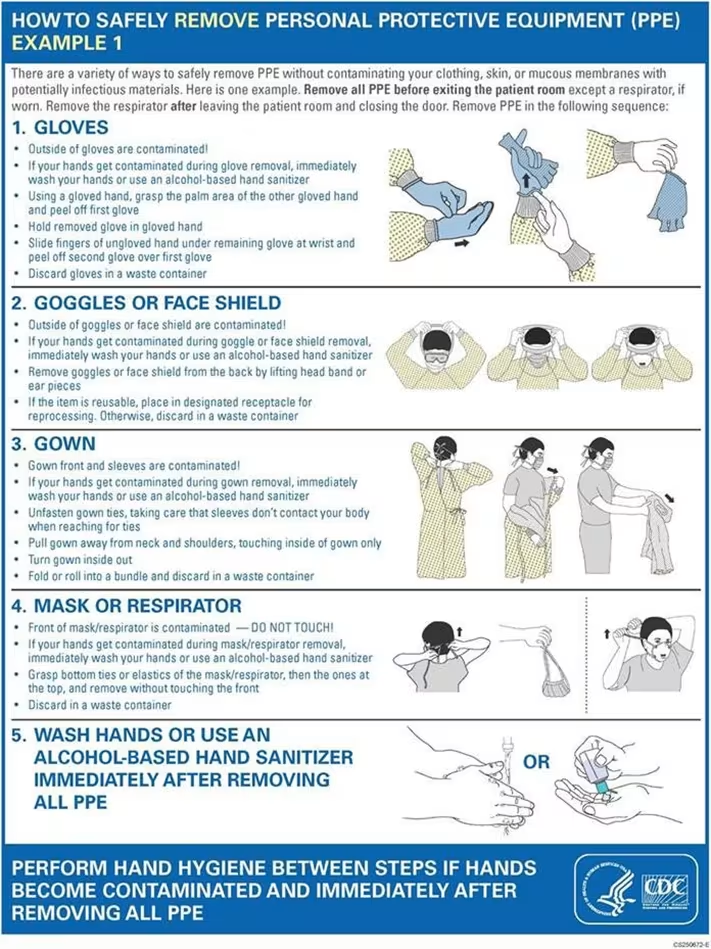
Sequence For Putting On Personal Protective Equipment (PPE)31
CDC has recommended step by step procedure for wearing and removing PPE which is called donning and doffing procedures as mentioned in the figures below.